Improving Sleep and Enhancing Overall Health for Central Sleep Apnea (CSA) Patients
What is Sleep Apnea?
There are different types of sleep apnea, each with varying causes and treatments. The most common form is “obstructive sleep apnea” (OSA), in which breathing is obstructed by a narrowing or blockage of the airway.
Another form of sleep apnea, “central sleep apnea” (CSA), stems from a problem with brain function, not an anatomical blockage. In CSA, the brain does not properly signal the respiratory muscles to stimulate a regular breathing pattern.1 While CSA is a less common and less studied form of sleep apnea, it’s just as serious as OSA.
Many people associate sleep apnea with symptoms like loud snoring or excessive sleepiness during the day. What’s less known about this underdiagnosed and undertreated condition is the profound connections that exist between sleep apnea and cardiac health.
How Sleep Apnea Negatively Impacts Cardiac and Overall Health
In recent years, physicians have increasingly recognized the links between sleep-disordered breathing and cardiovascular issues. As of 2022, the American Heart Association counts sleep among “Life’s Essential 8” ―lifestyle and health factors that contribute to optimal heart health. Good quality sleep protects the body by lowering blood pressure, keeping oxygen steady, lowering inflammation, and improving brain function, which can lead to healthy lifestyle decisions that protect the heart.
Sleep apnea not only increases the risk of cardiovascular disease, it can lead to worse outcomes for patients with cardiovascular disease. 2 For example, untreated CSA results in low oxygen levels, which are linked to high blood pressure, abnormal heart rhythm, heart attack, and even death.3 Many patients with CSA also have heart failure and atrial fibrillation,3,4 and patients who have CSA and heart failure are at increased risk for hospitalizations and death.5,6
On a daily basis, CSA’s impact can take a toll on every aspect of life. Imagine relentlessly experiencing chronic fatigue, excessive daytime sleepiness, cognitive impairment, mood changes, and difficulty sleeping. The symptoms of untreated CSA take away the ability to enjoy normal activities and keep patients from feeling like themselves. Once CSA is diagnosed, treatment options are limited.
ZOLL’s Innovative CSA Treatment Solution
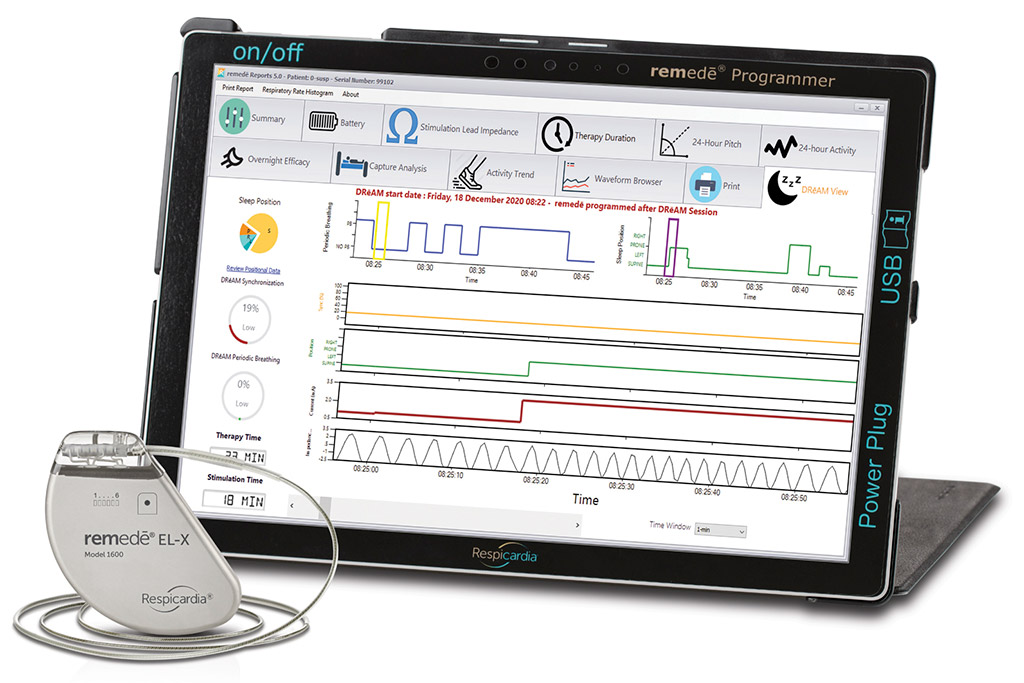
ZOLL’s remedē System is the only implantable device approved by the United States Food and Drug Administration (FDA) to treat moderate to severe CSA in adult patients. The remedē System, first approved by the FDA in 2017, activates automatically each night to stimulate the phrenic nerve in the chest, which sends signals to the diaphragm to help restore a more normal breathing pattern.1
The next-generation remedē EL System, approved by the FDA in 2021, combines enhanced functionality with a patient-friendly design, simplifying the implant procedure and providing greater device longevity for patients with CSA. Features include longer average battery life, reduced size, stimulation and sensing from a single lead, and respiration and device algorithm monitoring capabilities via DRēAM View, software which provides an expanded set of full-night, detailed data detected by the device.
All models of the remedē System are approved for conditional use with magnetic resonance imaging (MRI) by the FDA. Because it can be implanted on either side of a patient’s chest, the remedē System can also be used with another stimulation device such as a pacemaker.
Transforming Lives and Patient Impact
ZOLL’s remedē System is transformative for patients, both statistically and in providing a quality of life that was not possible without treatment. Of note, remedē patients:
- Experienced a 96% reduction in Central Apnea Index at 1 year7
- 78% of reported improved quality of life using the Patient Global Assessment8
- 95% said they would elect to have the procedure again8

Patients have shared their experiences living with CSA and how the remedē System has improved their lives―impact best heard directly.
Shawn Johnston, a proud father of two active boys from Missouri, was experiencing a serious and unexplained decline in overall health. “My health was getting worse and worse every day,” he said. “I felt like there was nothing I could do about it.” After years of interrupted sleep, lethargy, concentration problems and other symptoms, Shawn was diagnosed with central sleep apnea and received the remedē System.
“Once the device was activated, it was the first time I slept in 10 years. Now that I have the remedē System my life is completely different. I have the energy to take care of my kids. I am more lively, I am able to focus, keep up with my job, exercise, and feel like a normal person. The device has given me my life back,” said Shawn.

Larry Pigeon of Viginia said, “I was tired all the time, difficult to get along with and depressed because of my health…The first night with remedē I got sleep like I never had before. I just feel better, and I am active and busy, and I think better.”
The harm of untreated CSA impacts those closest to patients. After receiving the remedē System, Larry said, “My wife gets to sleep – she doesn’t have to stay awake and monitor me.”
Another remedē System recipient, Alex DeLeon of Texas, shared, “I went from doing nothing to going back and having a life. Before I was absolutely not functioning at all. It has been a life changing device for me and my family.”
Click here to discover more about remedē patient experiences.
1. Costanzo M.R., et al. The Lancet. 2016;388:974–82.
2. “Sleep Apnea and Heart Health.” www.Heart.Org, 29 July 2024, www.heart.org/en/health-topics/sleep-disorders/sleep-apnea-and-heart-disease-stroke.
3. Oldenburg O, et al. Eur J Heart Fail 2007; 9:251-257.
4. Bekfani T, Abraham WT. Europace. 2016;18(8):1123–34. Epub 2016 May 26.
5. Khayat R, et al. J Card Fail. 2012;18:534–40.
6. Khayat, R et al. European Heart J. 2015;36 1463–69.
7. Costanzo MR, Ponikowski P, Javaheri S, et al. Sustained Twelve Month Benefit of Phrenic Nerve Stimulation for Central Sleep Apnea. Am J Cardiol. 2018. pii: S0002-9149(18)30258-3. doi: 10.1016/j.amjcard.2018.02.022.
8. Costanzo MR, Javaheri S, Ponikowski P, et al. Transvenous Phrenic Nerve Stimulation for Treatment of Central Sleep Apnea: Five-Year Safety and Efficacy Outcomes. Nat Sci Sleep. 2021;13:515-526.